Getty Is dizziness a symptom of COVID-19 coronavirus?
Perhaps you’ve been suffering from dizziness, and now you’re wondering whether you have the novel coronavirus (COVID-19). Obviously, there’s no way to know for sure whether you have COVID-19 unless you can get tested, but tests aren’t always available in many areas.
Scientists are still learning about the virus, but there is a growing body of research that isolates which symptoms are commonly seen in people who have tested positive for COVID-19. In addition, national and world health organizations have released lists of symptoms. Is dizziness a symptom of coronavirus?
The answer is that dizziness doesn’t appear on the main symptom lists put out by the Centers for Disease Control and Prevention and the World Health Organization. It also doesn’t appear in some research studies. Thus, it’s certainly not one of the most common symptoms of COVID-19 (although it may be associated with other symptoms, such as nausea or headache.) However, dizziness has been reported as a symptom in some COVID-19 studies.
For example, the April 2020 study Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China listed dizziness as a symptom of COVID-19. This study found that some coronavirus patients reported having neurological problems. Dizziness was listed in that grouping. The study found:
Neurologic manifestations fell into 3 categories: central nervous system manifestations (dizziness, headache, impaired consciousness, acute cerebrovascular disease, ataxia, and seizure), peripheral nervous system manifestations (taste impairment, smell impairment, vision impairment, and nerve pain), and skeletal muscular injury manifestations.
That study found that patients with more severe versions of the infection were more likely to have neurologic manifestations. In this study, 36.4% have neurologic manifestations. Of those, 16.8% reported dizziness. Here’s a chart showing how those symptoms broke down. The first column, starting on left, is total with percent in brackets. The next column is for those with severe infection, and the third column is for those with non-severe infection.
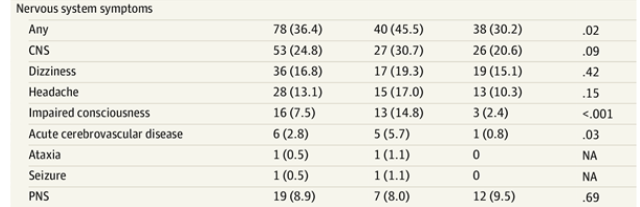
Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China
If you think you have COVID-19, you should check with your primary care doctor or call a coronavirus hotline. The Centers for Disease Control and Prevention says you should go to the hospital if you have:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
The CDC notes that you should seek medical attention if you have symptoms you find severe or concerning. Studies have found that some people with COVID-19 never have symptoms at all.
Context can also matter; having contact with a person who tested positive for COVID-19 or living in a COVID-19 geographic hotspot can also make it more likely that you’ve contracted the illness. You can find an updated map of COVID-19 cases in the United States here. You can also find testing data and maps and a listing of coronavirus drive-through testing sites by state. Here’s how to use Apple Maps to find coronavirus testing locations.
Here’s what you need to know:
The CDC Lists 9 Common Symptoms That Could Indicate a Coronavirus Infection & Dizziness Doesn’t Make the List
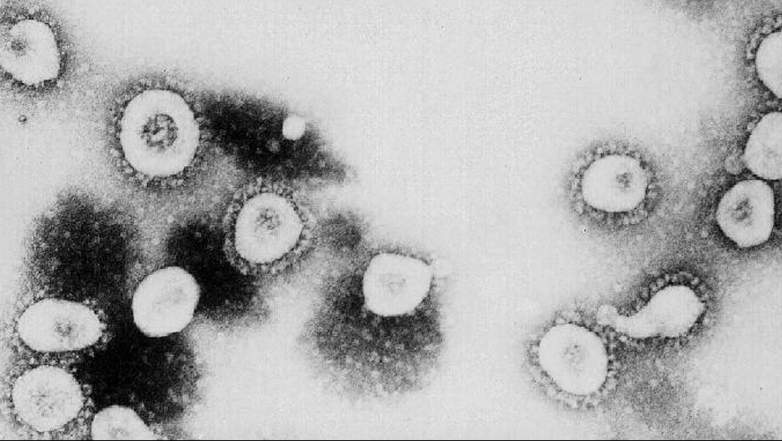
GettyThis photo from the Centers for Disease Control and Prevention shows a microscopic view of the coronavirus.
First of all, John Hopkins Medicine recommends you immediately seek medical treatment if you’re experiencing dizziness and these symptoms:
New confusion or trouble speaking or understanding speech
New slurred speech or hoarseness of voice
New numbness or weakness of the face, arm, or leg
New clumsiness or tremor (shaking) of the arms or legs
New trouble seeing out of one or both eyes, or to one side
New double vision or inability to move one or both eyes
New unequal pupils or drooping eyelid on one side
New inability to stand even when holding onto something firm
Sudden severe vomiting with no known cause
Sudden severe headache or neck pain with no known cause
COVID-19 isn’t the only cause that might be triggering dizziness. For example, dizziness could be a sign of a stroke.
The Centers for Disease Control and Prevention reports that people with COVID-19 “have had a wide range of symptoms reported – ranging from mild symptoms to severe illness.” These symptoms may appear 2-14 days after exposure to the virus. The CDC list doesn’t include dizziness:
- Fever
- Cough
- Shortness of breath or difficulty breathing
- Chills
- Repeated shaking with chills
- Muscle pain
- Headache
- Sore throat
- New loss of taste or smell
However, research studies have outlined other symptoms that didn’t make that list. Specifically, some of the other symptoms noted in research include diarrhea and other gastrointestinal issues, as well as red-rimmed eyes.
When should you decide to get tested? CDC advises:
Not everyone needs to be tested for COVID-19. Here is some information that might help you make decisions about seeking medical care or testing.
Most people have mild illness and are able to recover at home without medical care. They may not need to be tested. There is no treatment specifically approved for people who have COVID-19.
In a lengthy report on COVID-19, the World Health Organization listed these symptoms. The organization also did not include dizziness on that list:
Symptoms of COVID-19 are non-specific and the disease presentation can range from no symptoms (asymptomatic) to severe pneumonia and death. … Based on 55924 laboratory confirmed cases, typical signs and symptoms include: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), myalgia (muscle pain) or arthralgia (joint pain) (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%), and hemoptysis (0.9%), and conjunctival congestion (0.8%).
According to WHO, “People with COVID-19 generally develop signs and symptoms, including mild respiratory symptoms and fever, on an average of 5-6 days after infection (mean incubation period 5-6 days, range 1-14 days).”
The WHO advises that most people infected with COVID-19 virus “have mild disease and recover. Approximately 80% of laboratory confirmed patients have had mild to moderate disease.”
Research Studies Have Outlined a Variety of Symptoms That Could Indicate You Have Coronavirus

GettyMedical workers assist people standing in line at NYC Health + Hospitals/Gotham Health, Gouverneur waiting to be tested for the coronavirus (COVID-19) on April 24, 2020, in New York City.
Here’s a roundup of research studies into how coronavirus unfolds in some patients. These studies did not highlight dizziness as a symptom.
Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State
This study found that comorbidities were identified in 86% of cases, “with chronic kidney disease and congestive heart failure being the most common.” Initial symptoms “included shortness of breath (76%), fever (52%), and cough (48%).” The mean onset of symptoms before going to the hospital was 3.5 days, and 81% of patients were admitted to the ICU less than 24 hours after hospital admission.
Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study.
This study found that 51% of patients had chronic diseases. These symptoms were noted:
Patients had clinical manifestations of fever (82 [83%] patients), cough (81 [82%] patients), shortness of breath (31 [31%] patients), muscle ache (11 [11%] patients), confusion (nine [9%] patients), headache (eight [8%] patients), sore throat (five [5%] patients), rhinorrhoea (four [4%] patients), chest pain (two [2%] patients), diarrhoea (two [2%] patients), and nausea and vomiting (one [1%] patient) … 17 (17%) patients developed acute respiratory distress syndrome and, among them, 11 (11%) patients worsened in a short period of time and died of multiple organ failure.
The study noted that COVID-19 was “more likely to affect older males with comorbidities, and can result in severe and even fatal respiratory diseases such as acute respiratory distress syndrome.”
Clinical Characteristics of Coronavirus Disease 2019 in China
This study found that “the most common symptoms were fever (43.8% on admission and 88.7% during hospitalization) and cough (67.8%). Diarrhea was uncommon (3.8%). The median incubation period was 4 days.”
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
This study found that “(48%) patients had a comorbidity, with hypertension being the most common (58 [30%] patients), followed by diabetes (36 [19%] patients) and coronary heart disease (15 [8%] patients). Multivariable regression showed increasing odds of in-hospital death associated with older age.”
Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms
This study found that “smell and taste loss were reported in 68% (40/59) and 71% (42/59) of Covid-19-positive subjects, respectively, compared to 16% (33/203) and 17% (35/203) of Covid-19-negative patients. Smell and taste impairment were independently and strongly associated with Covid-19-positivity.”
This is a good roundup of research studies into COVID-19.
READ NEXT: The Real Story of Waco