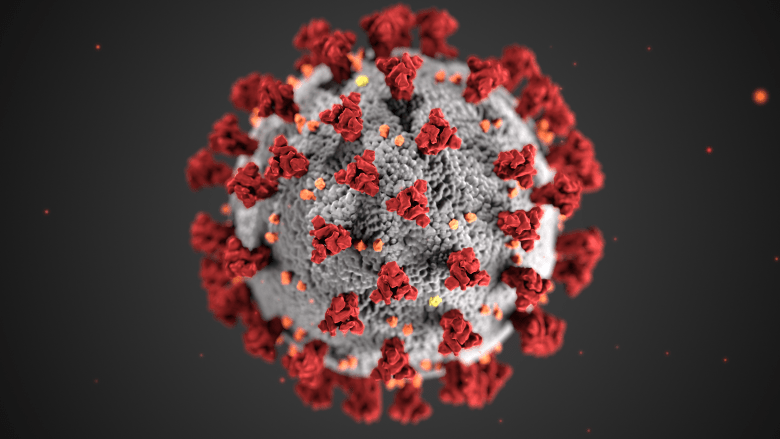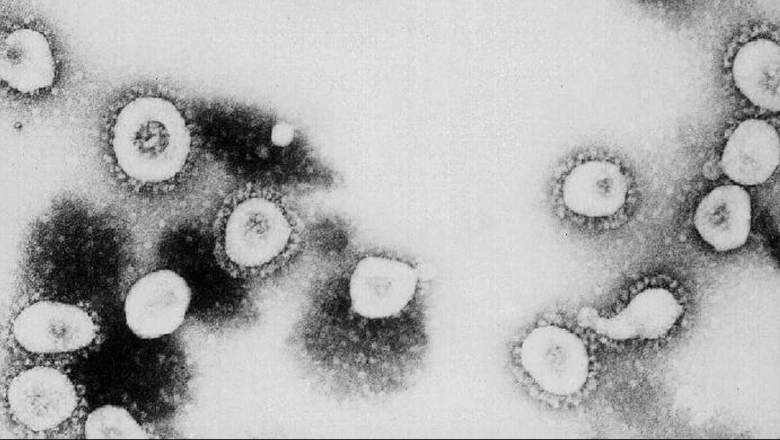
GEtty This undated handout photo from the Centers for Disease Control and Prevention (CDC) shows a microscopic view of the novel coronavirus.
An interview with Dr. Richard Bartlett has gone viral on Facebook recently. Bartlett claims in the interview that budesonide, commonly prescribed in the United States under the name Pulmicort, is a good treatment for COVID-19. Others doubt the coronavirus claims. Heavy spoke with several medical experts about budesonide and the science behind the claims.
The interview with Bartlett, from the Dallas-based TV show America Can We Talk?, has gone viral on Facebook. In the video, Bartlett says he had a lot of success treating his patients with inhaled, generic budesonide along with antibiotics to prevent secondary bacterial pneumonia. He says the medicine is being used in other countries, too. You can watch the interview below, which Heavy noted has been deleted on some other Facebook sources.
Budesonide is traditionally used for asthma symptoms to decrease the severity and frequency of asthma attacks. In the U.S., it is prescribed under the name Pulmicort. It’s a corticosteroid that is designed to prevent inflammation in the lungs, and it’s only available by prescription.
Here’s what you need to know about budesonide and COVID-19:
Inhaled Corticosteroids Might Be Beneficial, but ‘Cure’ Claims Are Premature & More Studies Are Needed
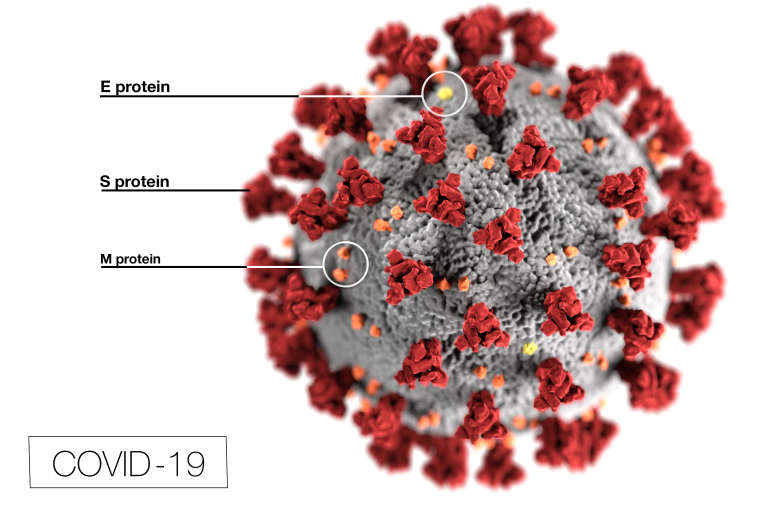
Dr. Michael Peters, MD, MAS, is an assistant professor in the School of Medicine at the University of California, San Francisco. He studies the impact of aerosolized/inhaled corticosteroids such as budesonide on ACE receptors. These ACE receptors are responsible for SARS-CoV-2, the novel coronavirus, entering human cells.
Peters warned against blanket claims about inhaled corticosteroids (ICS) preventing COVID-19. However, he also noted that these medications might indeed prove to be beneficial with further study.
“Inhaled corticosteroids are an effective and well-established treatment for asthma, but any claims regarding efficacy to treat or prevent the develop(ment) of Covid-19 infection are not supported by the currently available scientific data,” he said.
Peters added:
However, it is possible that ICS could be beneficial in CV19 disease and it is very reasonable to pursue clinical trials that test the potential for ICS to treat or prevent CV19 disease. There are currently multiple trials that have been developed to test this hypothesis, some of which are actively recruiting subjects. To my knowledge there is no data from randomized controlled trials for the efficacy of ICS for the treatment of CV19.
Peters said that any patient who is already on inhaled corticosteroids should continue the treatment as directed by their doctor.
“Most importantly, for patients already taking ICS there is no reason to suspect that ICS worsen CV19 disease and I would encourage all patients already on ICS to continue taking these medications,” he shared.
He noted that ICS might have some side effects, and that one trial indicated the corticosteroid dexamethasone might not be beneficial for patients who didn’t suffer severe COVID-19. So more studies are needed to know for certain how the medications will interact with COVID-19 in its various stages.
Peters said:
ICS do have some potential side effects, most commonly the development of thrust (a fungal throat infection), sore throat, hoarse voice, and in certain patient populations there is a slight increase in the risk of developing bacterial pneumonias. In addition, the recent Recovery trial that was conducted in the UK demonstrated that treatment with dexamethasone (a systemic corticosteroid) in patients not on oxygen might increase the risk of worse CV19 disease. So it is reasonable to be concerned that ICS could have negative consequences if given to non asthma patients without CV19 infection. Future studies need to be conducted to further understand these possible risks.
Inhaled Corticosteroids Come With Benefits & Risks With COVID-19, So Consult Your Doctor

GettyTouro University Nevada medical students Allison Boynton, Allison Moran and Claire Chen put on personal protective equipment as they get ready to conduct medical screenings.
Dr. Joi Lucas, MD, is a board-certified pediatric pulmonologist practicing in Orlando and Tampa, Florida. She told Heavy that Pulmicort is commonly used in children and infants as a nebulizer inhaled steroid treatment for asthma and chronic lung disease of prematurity.
She told Heavy about coronavirus: “COVID-19 has unique pathogenicity and is efficiently transmitted with few clinical symptoms by aerosolized droplets originating from the upper respiratory tract. Later in the disease course replication of the virus occurs in the lower respiratory tract with an attack of organs expressing the same receptor, ACE2, and overwhelming cytokine-induced inflammation.”
Pulmicort was introduced more than 25 years ago to treat asthma in children. The safety profile of the drug is well known, she said.
“Several placebo-controlled multicenter trials in the United States demonstrated the efficacy and tolerability of budesonide in children, adolescents, and adults for treating asthma,” she said. “Pulmicort in combination with long-acting albuterol is also used to successfully manage chronic obstructive pulmonary disease (COPD) … .”
Pulmicort hasn’t had some of the negative side effects that other inhaled steroids demonstrated, she noted.
“Fortunately, Pulmicort has not demonstrated side effects such as growth delay, decreased bone mineral density, or cataract formation commonly associated with other inhaled steroids, when it is used in short intervals,” Lucas told Heavy.
There are differing opinions about the use of steroids with COVID-19, since some steroids might decrease the body’s immune response. However, there is also evidence that some inhaled steroids might improve the outcome of COVID-19, so it’s best to simply ask your doctor, she shared.
“Of note, patients with COPD and asthma are at increased risk for severe infection with COVID-19,” she said. “Steroids suppress immune response mitigating inflammation, but also potentially dampen … the body’s natural defenses against invading viruses like COVID-19. Some studies show use of inhaled corticosteroids in patients with asthma and COPD is associated with increased risk of upper respiratory tract infections. However, there is evidence to support specifically with some coronaviruses improved outcome with use of inhaled steroids. … Until the definitive benefits or risks of Pulmicort in the treatment of COVID-19 are known, patients should check with their doctor to determine if Pulmicort is a safe medication to use for COVID-19 symptoms.”
The Corticosteroid Dexamethasone Is Helping & Budesonide Targets the Lungs More Directly
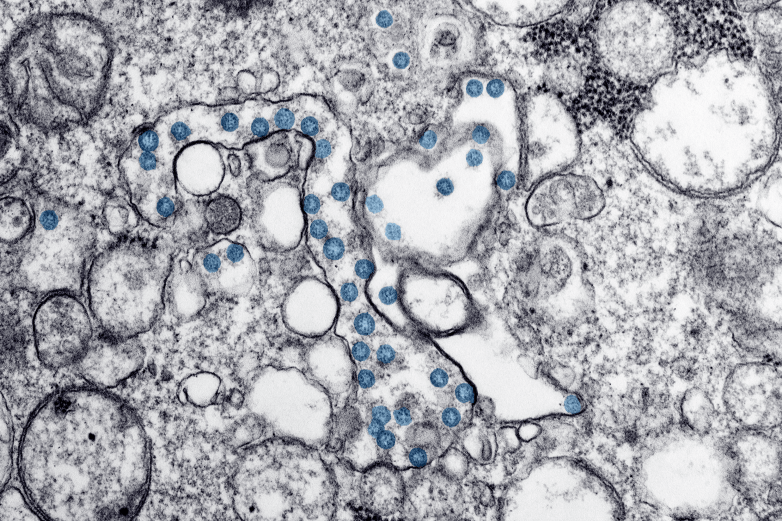
CDCTransmission electron microscopic image of an isolate from the first U.S. case of COVID-19, formerly known as 2019-nCoV. The spherical viral particles, colorized blue, contain cross-section through the viral genome, seen as black dots.
Dr. Don L. Goldenberg, emeritus professor of medicine at Tufts University School of Medicine, also spoke with Heavy about budesonide. Goldenberg shared that another corticosteroid has shown positive results in helping severely ill patients. But with so little known about budesonide’s role, it’s best to only take the medicine under the direction of a doctor.
Goldenberg shared:
Budenoside is a corticosteroid used orally or by nasal inhalation. Last month, studies from the University of Oxford demonstrated that another corticosteroid, dexamethasone, improved the survival of severely ill patients with COVID-19 infection. Dexamethasone, delivered orally or intravenously, has systemic absorption. All corticosteroids block inflammation and interfere with immune activation, two key processes of viral morbidity and mortality.
He shared that inhaled corticosteroids do let the drug target lung activity more directly, but current results are anecdotal.
“Inhaled corticosteroids have the advantage of more direct nasal and lung activity with potentially less adverse systemic side effects,” he said. “However, there are no randomized clinical trials and only anecdotal evidence of efficacy of nasal steroids in COVID-19 infection. Until then, such medications should only be used for potential or active COVID-19 infection under a physician’s supervision or as part of a clinical trial.”
Controlled Studies of Budesonide Are Needed to Determine the Risks & Benefits of Using the Medicine
Dr. Leann Poston, MD, is a licensed physician who also holds an MBA and an M.Ed. She’s currently a professional content contributor for Invigor Medical. In her career, she’s practiced medicine, acted as assistant dean and director of admissions at Wright State University Boonshoft School of Medicine and written articles for medical journals.
Poston told Heavy that the main risk from budesonide is suppressing the immune system, although it doesn’t do this to the same degree as oral steroids. She said that controlled studies on its effect on COVID-19 are needed since it’s unclear if the medicine would over-suppress the immune system or not.
“Budesonide is an inhaled corticosteroid,” she told Heavy. “Its purpose is to decrease inflammation and prevent an overreaction of the immune system (cytokine storm). Its risks are that it may suppress the immune system, though not to the extent that using oral steroids would. These competing factors, blunt an overreactive immune response versus suppressing the immune system, emphasize the need for controlled studies before claiming that the drug helps or harms patients with COVID.”
She told Heavy that one laboratory study found that budesonide may have some inhibitory actions on COVID-19, but more study needs to be done.
“A recent study has shown that in a laboratory setting pretreatment of respiratory cells with budesonide, in combination with glycopyrronium and formoterol, has inhibitory actions on COVID replication and cytokine production,” Poston said. “The study concludes that there is currently no evidence either for or against the benefit of using inhaled corticosteroids for the treatment of COVID.”
However, patients already taking inhaled corticosteroids for asthma or COPD will likely want to continue their medication.
“Patients already on inhaled corticosteroids for asthma or COPD should consult their health care provider,” she said. “However, in most cases, withdrawal of inhaled corticosteroids at the onset of a respiratory virus is more likely to be harmful than good.”
As you can see, the science is still open when it comes to Budesonide and more studies are needed. If you have COVID-19 symptoms and are wondering about Budesonide, your best course of action is to talk to your doctor about whether it might be beneficial to try or not.
READ NEXT: Daily COVID-19 Updates