
Getty How can you know if you have coronavirus?
Many of us have been there. You or a loved one are just feeling off, and you’re wondering how you can know if you have the novel coronavirus (COVID-19). Obviously, there’s no way to know for sure unless you can get tested, but tests aren’t widely available in many areas.
However, there’s a growing understanding of what COVID-19 symptoms look like (you’ll find more details of them throughout this article). Although the symptoms can resemble the flu or even a common cold, researchers are starting to get a better understanding of how coronavirus unfolds. If you think you have COVID-19, you should check with your primary care doctor or call a coronavirus hotline. The Centers for Disease Control and Prevention says you should go to the hospital if you have:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to wake or stay awake
- Bluish lips or face
The CDC notes the list of symptoms is not all-inclusive, and you should seek medical attention if you have symptoms you find severe or concerning. Studies have found that some people with COVID-19 never have symptoms at all. Thus, the only way to know for sure is to get a test, which can be tough to come by in many areas.
The CDC has a full page devoted to the similarities and differences between COVID-19 and the flu, which you can find here. One key symptom seen in some COVID cases but not with the flu: “change in or loss of taste or smell.” CDC also notes, “If a person has COVID-19, they may be contagious for a longer period of time than if they had flu.”
According to CDC, “While COVID-19 and flu viruses are thought to spread in similar ways, COVID-19 is more contagious among certain populations and age groups than flu. Also, COVID-19 has been observed to have more superspreading events than flu. This means the virus that causes COVID-19 can quickly and easily spread to a lot of people and result in continuous spreading among people as time progresses.”
Context can also matter; having contact with a person who tested positive for COVID-19 or living in a COVID-19 geographic hotspot can also make it more likely to contract the illness. You can find an updated map of COVID-19 cases in the United States here. You can also find testing data and maps and a listing of coronavirus drive-through testing sites by state. Here’s how to use Apple Maps to find coronavirus testing locations.
Here’s what you need to know:
The CDC Lists 11 Common Symptoms That Could Indicate a Coronavirus Infection
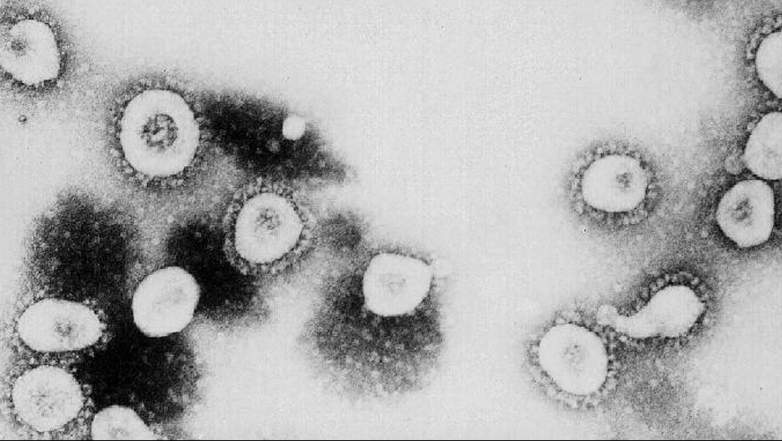
GettyThis photo from the Centers for Disease Control and Prevention shows a microscopic view of the coronavirus.
The Centers for Disease Control and Prevention reports that people with COVID-19 “have had a wide range of symptoms reported – ranging from mild symptoms to severe illness.” These symptoms may appear 2-14 days after exposure to the virus:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or small
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrea
However, those aren’t the only symptoms reported in research studies that investigated patients with the disease. Specifically, other symptoms noted include red-rimmed eyes.
CDC notes, “Anyone can have mild to severe symptoms. Older adults and people who have severe underlying medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness.”
When should you decide to get tested? CDC advises:
Not everyone needs to be tested for COVID-19. Here is some information that might help you make decisions about seeking medical care or testing.
Most people have mild illness and are able to recover at home without medical care. They may not need to be tested. There is no treatment specifically approved for people who have COVID-19.
In a lengthy report on COVID-19, the World Health Organization listed these symptoms:
Symptoms of COVID-19 are non-specific and the disease presentation can range from no symptoms (asymptomatic) to severe pneumonia and death. … Based on 55924 laboratory confirmed cases, typical signs and symptoms include: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), myalgia or arthralgia (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%), and hemoptysis (0.9%), and conjunctival congestion (0.8%).
According to WHO, “People with COVID-19 generally develop signs and symptoms, including mild respiratory symptoms and fever, on an average of 5-6 days after infection (mean incubation period 5-6 days, range 1-14 days).”
The WHO advises that most people infected with COVID-19 virus “have mild disease and recover. Approximately 80% of laboratory confirmed patients have had mild to moderate disease.”
Research Studies Have Outlined a Variety of Symptoms That Could Indicate You Have Coronavirus

GettyMedical workers assist people standing in line at NYC Health + Hospitals/Gotham Health, Gouverneur waiting to be tested for the coronavirus (COVID-19) on April 24, 2020, in New York City.
Here’s a roundup of research studies into how coronavirus unfolds in some patients:
Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State
This study found that comorbidities were identified in 86% of cases, “with chronic kidney disease and congestive heart failure being the most common.” Initial symptoms “included shortness of breath (76%), fever (52%), and cough (48%).” The mean onset of symptoms before going to the hospital was 3.5 days, and 81% of patients were admitted to the ICU less than 24 hours after hospital admission.
Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study.
This study found that 51% of patients had chronic diseases. These symptoms were noted:
Patients had clinical manifestations of fever (82 [83%] patients), cough (81 [82%] patients), shortness of breath (31 [31%] patients), muscle ache (11 [11%] patients), confusion (nine [9%] patients), headache (eight [8%] patients), sore throat (five [5%] patients), rhinorrhoea (four [4%] patients), chest pain (two [2%] patients), diarrhoea (two [2%] patients), and nausea and vomiting (one [1%] patient) … 17 (17%) patients developed acute respiratory distress syndrome and, among them, 11 (11%) patients worsened in a short period of time and died of multiple organ failure.
The study noted that COVID-19 was “more likely to affect older males with comorbidities, and can result in severe and even fatal respiratory diseases such as acute respiratory distress syndrome.”
Clinical Characteristics of Coronavirus Disease 2019 in China
This study found that “the most common symptoms were fever (43.8% on admission and 88.7% during hospitalization) and cough (67.8%). Diarrhea was uncommon (3.8%). The median incubation period was 4 days.”
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
This study found that “(48%) patients had a comorbidity, with hypertension being the most common (58 [30%] patients), followed by diabetes (36 [19%] patients) and coronary heart disease (15 [8%] patients). Multivariable regression showed increasing odds of in-hospital death associated with older age.”
Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms
This study found that “smell and taste loss were reported in 68% (40/59) and 71% (42/59) of Covid-19-positive subjects, respectively, compared to 16% (33/203) and 17% (35/203) of Covid-19-negative patients. Smell and taste impairment were independently and strongly associated with Covid-19-positivity.”
This is a good roundup of research studies into COVID-19.
Coronavirus Survivors Have Described Their Symptoms
Elizabeth Schneider is a woman living in Washington state who survived COVID-19. She wrote about the symptoms on Facebook:
First how easily you can get it. I believe I caught it when attending a small house party at which no one was coughing, sneezing or otherwise displaying any symptoms of illness. It appears that 40% of the attendees of this party ended up sick. The media tells you to wash your hands and avoid anyone with symptoms. I did. There is no way to avoid catching this except avoiding all other humans. 40% of folks were all sick within 3 days of attending the party all with the same/similar symptoms including fever.
Second, the symptoms appear to be different depending on your constitution and/or age. Most of my friends who got it were in their late 40s to early 50s. I’m in my mid 30s. For us it was headache, fever (for first 3 days consistently and then on and off after 3 days), severe body aches and joint pain, and severe fatigue. I had a fever that spiked the first night to 103 degrees and eventually came down to 100 and then low grade 99.5. Some folks had diarrhea. I felt nauseous one day. Once the fever is gone some were left with nasal congestion, sore throat. Only a very few of us had a mild itchy cough. Very few had chest tightness or other respiratory symptoms. Total duration of illness was 10-16 days. The main issue is that without reporting a cough or trouble breathing many of us were refused testing. I tested positive through the Seattle Flu Study. This is a RESEARCH study here in Seattle and they have been testing volunteers for strains of the flu to study transmission within the community. A few weeks ago, they started to test a random subset of samples for COVID-19 infection. They sent my sample to the King County Public Health Department for confirmation; however, I was told that all of the samples that have tested positive in the research study have been confirmed by Public Health.
UPDATE: I called King County Public Health and they said that they aren’t doing secondary tests and that if you test positive anywhere in King County, whether the flu study or not, you have tested positive. A total of 7 other people from the party have tested positive. 2 from a doctor’s office and the rest from the flu study.
As of Monday March 9th, it has been 13 days since my symptoms started and more than 72 hours since my fever subsided. The King County Public Health Department is recommending you stay isolated for 7 days after the start of symptoms or 72 hours after your fever subsides. I have surpassed both deadlines so I am no longer isolating myself however I am avoiding strenuous activity and large crowds and I obviously will not come near you if I see you in public. I was not hospitalized. Not every country is hospitalizing everyone with a COVID-19 infection and in my case, and in many other cases, I didn’t even go to the doctor because I was recovering on my own and felt it was just a nasty flu strain different from the ones I have been protected from with this season’s flu vaccine.
I also truly believe the lack of testing is leading to folks believing that they just have a cold or something else going out into public and spreading it. And worse folks with no symptoms are also spreading it as in the case of a person attending a party or social gathering who has no symptoms.
Danielle Nelson is a Wisconsin woman who survived COVID-19. She wrote on Facebook:
I am a generally healthy person. I have no underlying health conditions. Before March, I had never spent a night in a hospital bed. About 3 weeks ago, I started having chest pain. I self-quarantined but I wrote it off as anxiety. About 2.5 weeks ago, I got a fever. Despite regular Tylenol and ice packs, it could not be controlled. After a week of this and sleeping 20 hours a day, I went to the ER. They tested me and sent me home. A few days later I barely had the energy to get to the bathroom. I was so tired and winded. I went back to the ER and was admitted.
For the week I was in the hospital I had to have help going to the bathroom. The doctors were having a hard time controlling my fever. I slept covered in ice packs. My blood pressure was dangerously low. I was getting IV fluids because I was severely dehydrated. I could barely eat. I was on oxygen because I had a hard time breathing due to the pneumonia and fluid in my lungs. I feel so lucky I didn’t need a ventilator. When I had moments of physical relief, I sobbed. I tried to focus on my meditation app. I tried to reply to texts. I reflected on my life. I told my mom and Patrick I loved them.
I was released from the hospital 4 days ago but it’s not over. I am tired. I can do a little something and then have to rest. In fact, I write this with my head on a pillow.
She has also written extensively about her experiences here.
Others who have survived and shared lengthy descriptions of symptoms on Twitter include David Lat, Chris Gough and Dr. Yale Tung Chen.
According to NBC News, coronavirus is a virus with a “slow burn,” and experts say that, “very often,” the earliest symptoms are “minor physical complaints — slight cough, headache, low-grade fever,” that gradually get worse. Loss of taste and smell and red-rimmed eyes have also emerged as possible symptoms of COVID-19. It often takes about a week after symptoms start to know whether the virus will worsen or the person will just get better, experts say. About half of people who have COVID-19 never get symptoms at all, according to Fox News. That detail is based on research studies in Iceland, Italy and the Diamond Princess cruise ship.
READ NEXT: The Real Story of Waco